Impact of eReferral on reducing the burden of treatment for patients
The Burden of Treatment Theory explains how patients are tasked with taking on responsibility for managing their illness, which places added demands and workload burden on them.1 As these demands and burdens accumulate, some patients may become overwhelmed, resulting in adverse healthcare outcomes. Studies have revealed that that burden of navigating the system can lead to care delays or even deter patients from seeking necessary care.2
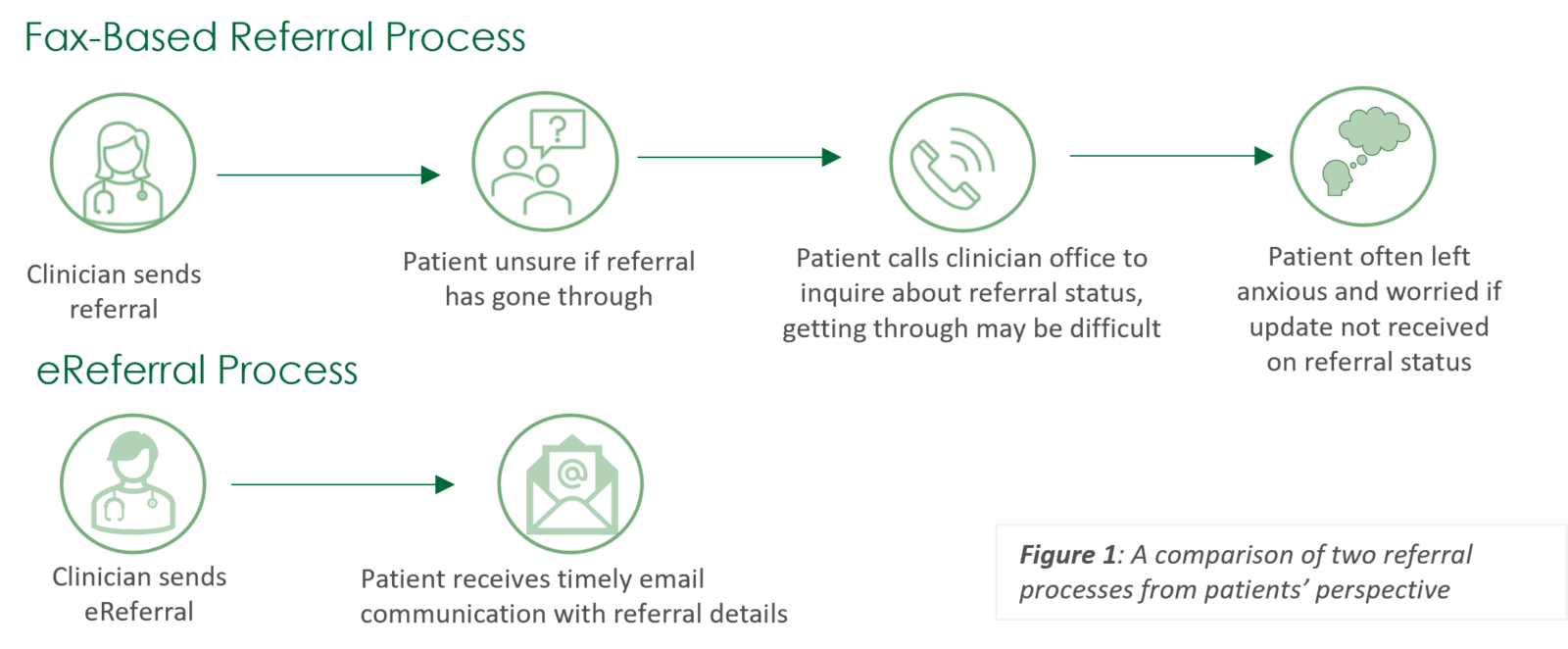
The patient burden associated with fax referrals underscores the challenges and inconveniences patients face when healthcare providers rely on fax machines to exchange referral information. This referral method can lead to numerous obstacles, such as additional administrative responsibilities for patients, and a sense of disconnection from their own healthcare. These burdens underscore the pressing need for healthcare systems to transition to more efficient means of referral methods that keep the patient informed along the way.
Key takeaways
eReferral has contributed to decreasing the burden of treatment for patients, easing administrative responsibilities and reducing anxiety associated with navigating healthcare services.
Decreased Burden of Treatment
To investigate how eReferral (electronic referral) influences the patient experience, in-depth interviews were conducted with five patients referred for various medical appointments by their primary care physicians, including breast mammography, ultrasounds, and mental health therapy. This case study highlights the emerging trend of decreased treatment burden for patients, providing valuable insights into the advantages of utilizing eReferral.
Several patients noted that eReferral significantly relieved the burden associated with the referral process by streamlining and simplifying the patient experience. When using fax-based referral methods, patients often faced the challenge of having to repeatedly contact the clinician’s office to obtain information about the status of their referral. This caused uncertainty and anxiety, particularly when dealing with serious and complicated medical issues. With eReferral, patients shared how they no longer needed to worry about making time-consuming phone calls or waiting for callbacks to confirm the status of their referral. Instead, they could easily access their referral details via email. One patient, who was struggling with mental health illness, recounted a particularly challenging period in their life and emphasized how eReferral had provided a lifeline during that crisis. The speed and seamlessness of eReferral eliminated the legwork often associated with fax-based referral methods. The patient also indicated that the swift delivery of the referral information validated their mental health concerns.
It (eReferral) was like magic. I was in the deepest, darkest place in my life and eReferral made getting help seamless. I went from my doctor’s office to the mental health clinic, so I could start healing. There was no in between of me doing any leg work. I didn’t need to worry about what was happening behind the scenes because I received the communication. It was so smooth and straightforward. It was exactly what I needed at the right time.
Patient
Struggling with mental health illness
Acknowledgements
The Ontario eServices Program delivers digital services (eConsult and eReferral are the
first initiatives in the scope of the program) that support clinical workflows and facilitate smoother transitions in care and an improved patient experience. The Ontario eServices Program is co-led by the Ontario eConsult Centre of Excellence (eConsult COE) and the eHealth Centre of Excellence (eCE) and is funded by Ontario Health.
1May, C. R., Eton, D. T., Boehmer, K., Gallacher, K., Hunt, K., MacDonald, S., Mair, F. S., & May, C. M. (2014, June). Rethinking the patient: using Burden of Treatment Theory to understand the changing dynamics of illness. BMC Health Services Research, 14(281). https://bmchealthservres.biomedcentral.com/articles/10.1186/1472-6963-14-281
2Kyle, M. A., & Frakt, A. B. (2021). Patient administrative burden in the US health care system. Health services research, 56(5), 755–765. https://doi.org/10.1111/1475-6773.13861
Interested in learning more?
Interested in partnering with us or learning more about
what we can offer you? Please reach out here.
Get the latest resources and insights
-

Plain Language Description: Ocean eReferral to Telus CHR
Amplify Care and Telus Health have partnered to allow healthcare clinicians to send and receive…
-

How AI Scribes are reducing administrative burden in primary care
Learn more about an evaluation that shows AI scribes are alleviating the administrative burden on…
-

eReferral email notifications enhance patient experience
Patient email notifications sent by the eReferral solution result in patients feeling more informed and…
-

Webinar on improving access and experience of care for patients
Sharing some tips, tricks, and key takeaways from our Ideal Primary Care Practice Model webinar,…