eConsult: A case study on eConsult use in primary care to enable timely patient care with confidence
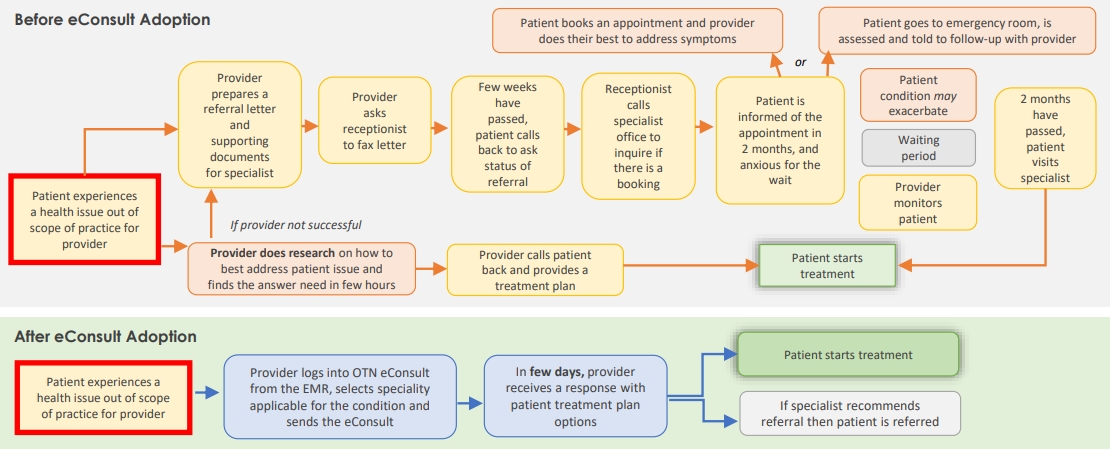
The median wait time from primary care provider referral to consultation with a specialist in Ontario is 6.7 weeks, and an additional 8.6 weeks from seeing a specialist to treatment.¹ The long waits are concerning as patients often “face the greatest wait-related risk at the earlier phases of care before disease has been conclusively diagnosed and a treatment plan established.”² The current referral process is known to be a common cause of frustration, with primary care providers reporting difficulties in finding an available specialist, not receiving confirmation of receipt of referral, not being informed of appointment, and receiving no information for follow-up treatment.³
Key takeaways
When patients present with issues outside the scope of practice for the primary care provider, eConsult enables timely access to experience-based specialist knowledge, increasing primary care provider confidence in developing a treatment plan, facilitating better patient outcomes and reducing the need for specialist referrals.
The availability of eConsult, an asynchronous communication between healthcare providers and specialists that occurs through Ontario Telemedicine Network (OTN), has been shown to be promising in addressing such issues.⁴ Dr. Rebecca Lubitz, a primary care provider in Kitchener, Ontario, adopted eConsult in her practice in November 2016. She uses eConsult approximately twice a month to support timely patient care for issues outside her scope of practice that in the absence of eConsult would have resulted in conducting extensive research to support a treatment plan and perhaps making a referral for a specialist consult.
A patient with a skin rash was frustrated with how long the rash was taking to resolve and wondered if something other than standard treatments can be done. I used eConsult to connect with a dermatologist, sent them a picture of the rash (taken with my cellphone) and asked if my diagnosis, treatment plan, and time to resolution were accurate. The dermatologist reassured me that the diagnosis and treatment plan were appropriate. This allowed me to reassure the patient, and the patient felt better about the plan.
Dr. Rebecca Lubitz
Andrew Street Family Health Centre
With eConsult, there is increased…
- patient satisfaction and confidence in primary care provider
- ability to have questions answered that would normally require a great deal of research for a problem that may not seem serious enough to warrant a referral, saving the provider time
- primary care provider confidence in the care plan
- appropriate referrals received from primary care providers
- easy access to over 500 specialists across Ontario, in over 100 specialties
- fast response (2.5 days average in Waterloo Wellington)
- Providers’ ability to provide timely care for patients, based on experience-based knowledge from specialists
- learning opportunity to expand scope of practice
With eConsult, there is reduced…
- time to treatment
- likelihood of patient experiencing negative outcomes from progression of condition while waiting
- patient anxiety related to delay in treatment
- referrals to specialist when primary care provider is unsuccessful at finding information and a referral is seen as the best option at the time
- need to fax referrals, follow-up calls
- number of patients that provider needs to follow up with, as they wait for specialist visits
- patient travel costs
Case #1
An immunocompromised transplant patient developed back pain. An X-ray suggested osteomyelitis and a follow-up MRI was concerning but not diagnostic. The radiologist suggested an MRI with a certain contrast agent to make a more definitive diagnosis, but the patient’s specialist felt this agent was unsafe. The next steps in assessing whether this patient needed more aggressive treatment were thus unclear.
Waiting to see an orthopedist for a non-specific imaging finding would likely have taken months, which could have put the patient at risk. An eConsult was sent to an orthopedic surgeon who suggested monitoring ESR (erythrocyte sedimentation rate) and CRP (C-reactive protein) inflammatory markers, which would likely rise if an infection was brewing.
By suggesting a nonstandard approach (monitoring inflammatory markers) to a common family medicine problem (back pain), the eConsult specialist provided an alternate and safe plan to monitor this patient that I, as a family doctor, would have been hesitant to follow and may have been difficult to justify without specialist support.
Case #2
A complex homebound palliative patient with angina and severe aortic stenosis (a narrowed heart valve) had uncomfortable and ongoing chest pain. Seeing a specialist in person was not an option, as this patient was not physically able to leave the house without the aid of expensive medical transport the family could not afford.
Due to the patient’s severe heart valve narrowing, certain medications like long-acting Nitro, although standard in relieving angina pain, could dangerously drop his blood pressure and lead to falls or death, so I was hesitant to use this despite having few other options. The patient had long since declined surgical correction for the valve problem.
I consulted a cardiologist via eConsult who agreed that long-acting Nitro was reasonable despite the risks, since there were few other good options to make this patient comfortable. This reassurance from the cardiologist helped me reassure the family that I was indeed doing all that could be done. This specialist support provided the patient and family with some peace during a difficult time.
1Barua, B., Ren, F. (2016). Waiting Your Turn: Wait Times for Health Care in Canada, 2016 Report. Fraser Institute.
2CIHI (2016). Wait time for Priority Procedures in Canada, 2016. Ottawa, ON: CIHI.
3Canadian Medical Association (2012). Experience with Referrals: Results if two surveys.
4Vimalanandra et al. (2015). Electronic consultations (e-consults) to improve access to specialty care: a systematic review and narrative synthesis. Journal of Telemedicine and Telecare 21(6):323-30.
5OMD (2017). Provincial eConsult Initiative. at: ontariomd.ca.
Interested in learning more?
Interested in partnering with us or learning more about
what we can offer you? Please reach out here.
Get the latest resources and insights
-

Patient experience with eReferral Appointment Reminders
Patients who are emailed appointment reminders report a positive outcome from this service. Quick Facts…
-

eReferral Adoption Strategies throughout the COVID-19 Pandemic
Change Management Strategies during the Pandemic: Key takeaways Adapting change management tactics and clinical engagement…
-

A case study on a clinic’s experience using Online Appointment Booking for cervical cancer appointments and reminders for patients
Preventative care is a pillar of primary health care. Since the 1980s, there has been…
-

Impact of eReferral on patient efficiency and likelihood of referral appointment attendance
In a study conducted in Alberta, patients noted that the convenience of tracking referral information…