Supporting clinical best practices with an electronic referral system
Radiography is an appropriate cost-effective screening test for arthritis in older patients.¹ Evidence shows that although Magnetic Resonance Imaging (MRI) can provide detailed results for musculoskeletal derangement, it still detects clinically insignificant age-related degenerative changes, which may confound the results for older patients and affect the providers’ management plan.² Some clinicians refer older patients for unnecessary pre-consultation MRIs for knee pain. In older patients, the current underuse of radiography as an assistive tool in the diagnosis of knee pain, combined with the overuse of pre-consultation MRI, poses a substantial financial burden on Canada’s health care system.
Between 2003 and 2009, the number of MRIs performed in Canada doubled to 1.4 million per year,³ and is expected to continually increase as the population ages.⁴ According to the Health Council of Canada report, as many as 30% of MRIs were ordered unnecessarily in 2010.⁵ Huebner and colleagues conducted a chart review study to assess the impact of clinical decision support (DS) language embedded within the eReferral orthopedic form on the number of pre-consult MRIs ordered for knee pain patients ≥55 years referred to a local orthopedic clinic. The study reported a substantial reduction of 12% in the number of pre-consult MRIs when compared to findings from an earlier quality improvement study conducted at the same clinic.⁶
In other research the implementation of a DS tool at the point of order has been shown to reduce the total number of MRI imaging examinations by approximately 20 to 36%.7,8 It can be assumed that much of this reduction is due to the increased education available through the DS tools available for determining diagnostic imaging (DI) appropriateness. The use of the DI guidelines are sought to reduce the unwarranted imaging.9
The System Coordinated Access (SCA) Program, in collaboration with the Joint Department of Medical Imaging at the University Hospital Network in Toronto, have worked to integrate newly developed imaging guidelines into the eReferral form to assist referring physicians in making informed decisions regarding the ordering of DI.
Key takeaways
The integration of clinically validated guidelines for diagnostic imaging into the eReferral form supports clinical best practices for referring physicians
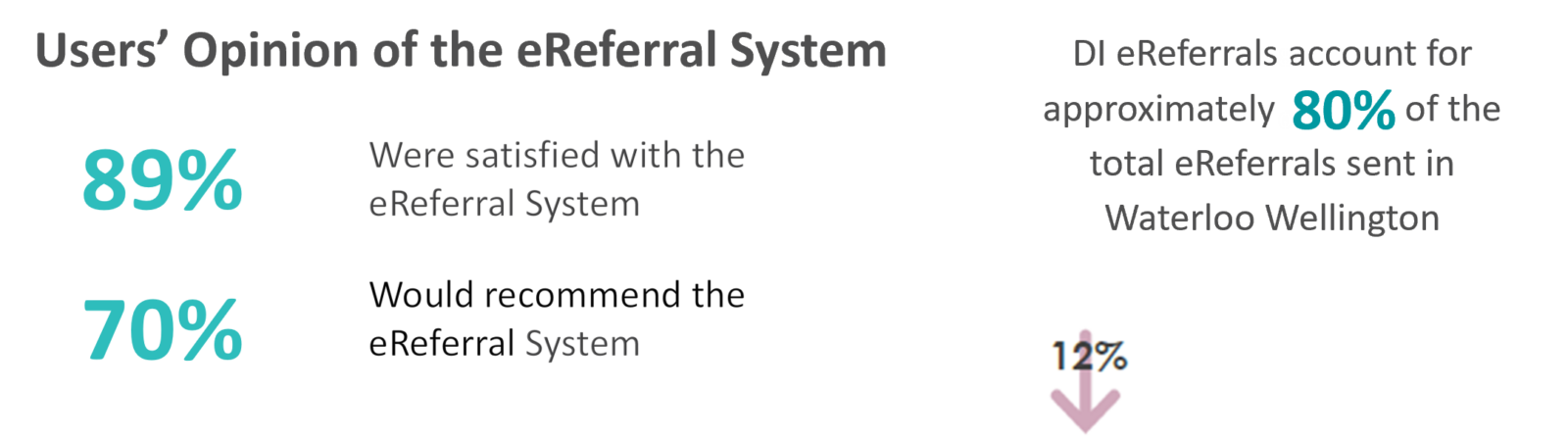
In March 2018, Waterloo Wellington (WW) LHIN hospitals started accepting eReferrals for DI services. Currently, DI eReferrals account for approximately 80% (28,299) of the total eReferrals processed in Waterloo Wellington.
Exploring clinicians’ opinion using a satisfaction survey
- Users who have adopted the eReferral solution and sent referrals electronically for more than six months received an invitation from the SCA Program to participate in a post-adoption satisfaction survey. The survey gathers users’ feedback on their experience with the system and the integrated guidelines as well as their perspective on its ability to support clinical best practices.
- With an overall response rate of 57% (sample size = 64) , the majority of participants (89%) were satisfied with the eReferral system. Most of the participants (70%) reported that they would recommend the eReferral solution. When users were asked about their opinion of the DI guidelines integrated in the eReferral form, the majority of users (90%) found it to be useful and 73% agreed /strongly agreed that it supports clinical best practices.
Exploring referring physicians’ opinion using a satisfaction question within the eReferral form
In October 2018, a satisfaction question was added to the eReferral form. This tool was introduced to collect clinicians’ feedback and capture the referring physicians’ opinions of the usefulness of the integrated guidelines. The response rate was 5% and the majority of respondents (80%) found the integrated guidelines to be very useful / useful in making decisions for DI referrals.
Acknowledgements
The Ontario eServices Program delivers digital services (eConsult and eReferral are the first initiatives in the scope of the program) that support clinical workflows and facilitate smoother transitions in care and an improved patient experience. The Ontario eServices Program is co-led by the Ontario eConsult Centre of Excellence (eConsult COE) and the eHealth Centre of Excellence (eCE) and is funded by the Ontario Ministry of Health (MOH).
- Braun H, Gold G. Diagnosis of Osteoarthritis: Imaging Bone. 2012 August ; 51(2): 278–288. doi:10.1016/j.bone.2011.11.019
- Petron D, Greis P, Aoki S, Black S, Krete D, Sohagia K, Burks R. Use of Knee Magnetic Resonance Imaging by Primary Care Physicians in Patients Aged 40 Years and Older. Sports Health 2010. 2(5):385
- Vallis, M. and H. Piccinini-Vallis, Achieving Patient-Centeredness in Obesity Management Within Primary Care Settings. Canadian Journal of Diabetes, 2015. 39: p. S12.
- Wang, L., et al., Utilization patterns of diagnostic imaging across the late life course: a population-based study in Ontario, Canada. International journal of technology assessment in health care, 2008. 24(04): p. 384-390.
- Keely, E., C. Liddy, and A. Afkham, Utilization, benefits, and impact of an e-consultation service across diverse specialties and primary care providers. Telemed J E Health, 2013. 19(10): p. 733-8.
Interested in learning more?
Interested in partnering with us or learning more about
what we can offer you? Please reach out here.
Get the latest resources and insights
-

eConsult and eReferral supporting the chronic pain pathway
One in five Canadians suffer from chronic pain1. Wait times for multidisciplinary chronic pain clinics…
-

Webinar on leveraging AI scribes for your ideal practice (part 1)
Sharing some tips, tricks, and key takeaways from our Ideal Primary Care Practice Model webinar,…
-

Fiscal year 20/21 eReferral highlights
eReferral has had a record year with impressive referral volumes, increases in use and expansion…
-

Upcoming Webinar: Optimizing Primary Care Efficiency Through IHP Integration and Team Collaboration
Our next webinar is happening next week! Co-hosted by Julia Hutton, NP and Teresa Wetselaar,…