Virtual Care: A case study on virtual visits from a psychiatrist perspective
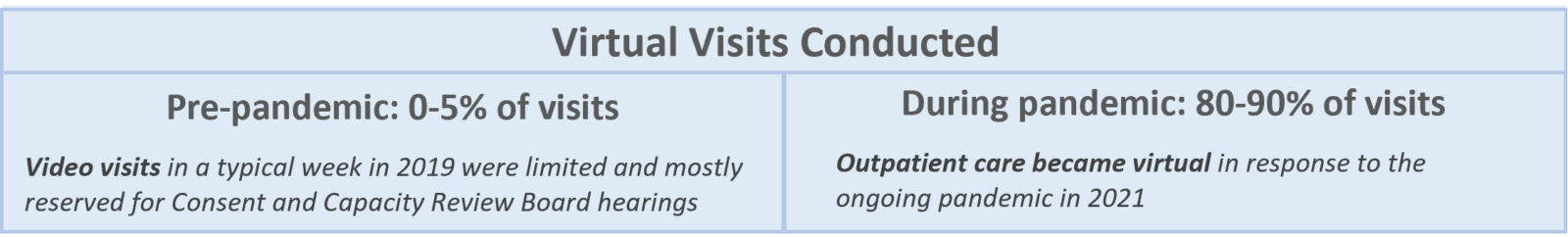
Virtual care in psychiatry can help to meet patients’ needs for convenient and accessible mental health services, providing an opportunity for immediate intervention and increased access to services for vulnerable individuals, while also increasing efficiency for clinics by reducing no-shows.1-3 However, although virtual delivery of treatment for depression and anxiety disorders has been known to achieve similar clinical outcomes to face-to-face support,4 systemic barriers have delayed a widespread implementation of virtual care for the delivery of mental health services.5 Prior to the COVID-19 pandemic, only 7% of psychiatrists delivered telepsychiatry and of the more than 48,000 Ontarians in need of psychiatric care, fewer than 1% saw a psychiatrist through virtual care.6
There is no doubt that the onset of COVID-19 played a role in accelerating the adoption of virtual care across the healthcare continuum. For example, the largest psychiatric hospital in Canada increased their virtual care capacity to over 850%, from 350 per month in March 2020 to almost 3,000 per month in April 2020.5 At Kaiser Permanente, 90% of psychiatric care is now delivered virtually.7 A survey of 20 American psychiatrists found that all of them changed to fully virtual practices in response to the pandemic, though most had not used telepsychiatry previously.8 For patients who either lack access to technology or broadband access and/or the cognitive ability to use video platforms, telephone (considered a virtual care modality) remains a necessary option when in-person restrictions are still in place.1
Key takeaways
Virtual care enables psychiatrists to provide continuity of care to patients, enabling provision of specialized mental health services to inpatient, outpatient, and community care, while facilitating integrated team-based care and communication between healthcare professionals.
Specialized mental health services are available for individuals with persistent mental health issues, patients transitioning from inpatient to gradual return to the community, seniors, and outreach consultation teams. With change management support from the eHealth Centre of Excellence, Dr. Kukreja, a psychiatrist in Kitchener, Ontario, adopted virtual care to support the delivery of specialized mental health services in response to the COVID-19 pandemic.
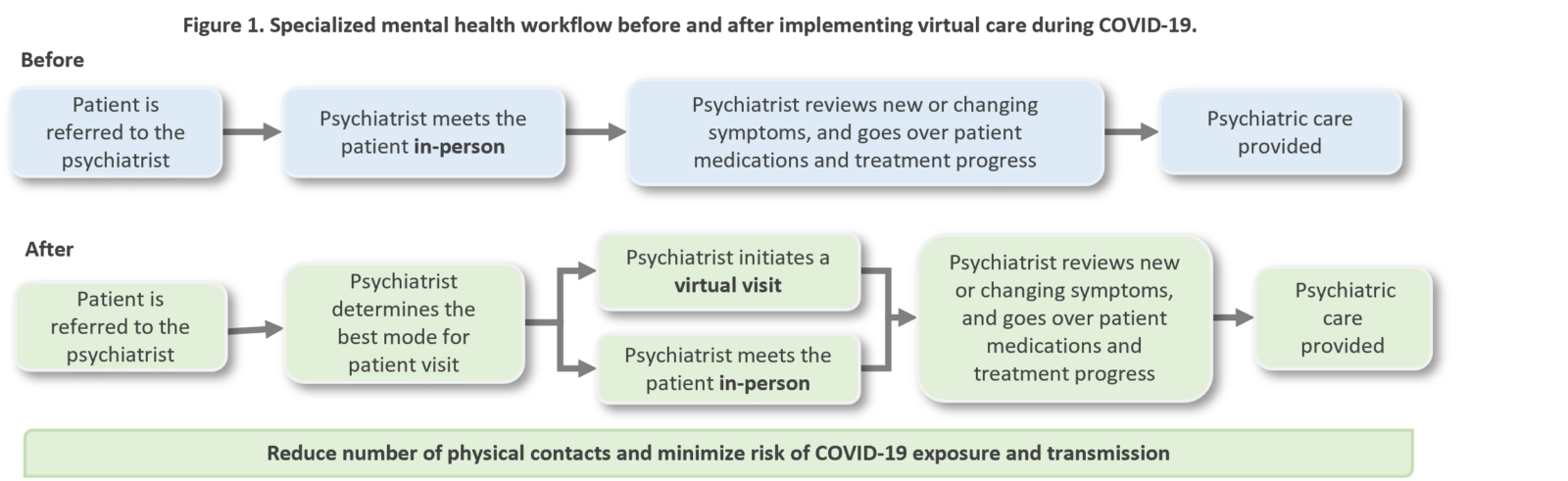
While an in-person appointment is vital in capturing the dynamics of the whole person in the initial encounter, virtual care has the potential to optimize follow-up visits and regular check-ins with patients, where it is appropriate. Virtual care does not replace in-person care for many specialized mental health services but when in-person visits are not available, telephone and video visits are great alternatives to providing care to patients who may not have received any care at all.
Dr. Kanwal Kukreja, Psychiatris
Kitchener, ON
Video visits enabled the psychiatrist to have a virtual face-to-face visit with patients, where appropriate, offer remote check-ins with patients from any location, as well as facilitate patient engagement during psychotherapy sessions and follow-up visits.
Dr. Kukreja’s reflection on the adoption and benefits of virtual visits to support mental healthcare needs noted:
Enhanced access to care for patients
- Patients that could not take time off work easily logged into their appointment on their mobile device
- Patients accessed care without concerns of infection or transmission of COVID-19
Improved health outcomes and quality of care through continuity of care
- Patients were enabled to conveniently address mental health concerns promptly rather than miss care, reducing the likelihood of missed appointments
- Proactive mental health management supported improved quality of care and outcomes for patients
Enhanced access to care for patients
- The psychiatrist connected virtually with other care professionals in a multidisciplinary team enabling the provision of integrated team-based care
In the recovery period of the pandemic, virtual care has the potential to support timely access to coordinated and integrated mental healthcare where appropriate, enhancing the capacity to respond to demands for specialized mental health services.
Key considerations were noted in adopting virtual care in psychiatry: technology use and comfort by the patient and staff, the quality of the relationship already established with the patient may impact suitability of virtual visits, requirements for physical assessments, integration of the virtual visits solution with documentation, scheduling and billing.
- American Psychiatric Association. (2021). Psychiatrists Use of Telepsychiatry During COVID-19 Public Health Emergency Survey Results.
- Whaibeh, E., Mahmoud, H. & Naal, H. Telemental Health in the Context of a Pandemic: the COVID-19 Experience. Curr Treat Options Psych 7, 198–202 (2020). https://doi.org/10.1007/s40501-020-00210-2
- Drerup, B. et al. (2021). Reduced No-Show Rates and Sustained Patient Satisfaction of Telehealth During the COVID-19 Pandemic. Telemed J E Health. doi: 10.1089/tmj.2021.0002.
- Kumar, V., et al. (2017). The Effectiveness of Internet-Based Cognitive Behavioural Therapy in Treatment of Psychiatric Disorders. Cureus 9(8):e1626. doi: 10.7759/cureus.1626
- Cisco Canada . CAMH enhances virtual capacity to respond to demand for mental health services. Cision News. 2020 May 4 [accessed 2021 Sep 13]. https://www.newswire.ca/news-releases/camh-enhances-virtual-capacity-to-respond-to-demand-for-mental-health-services-821323149.html.
- Serhal, E, Crawford, A, Cheng, J. Implementation and utilization of telepsychiatry in Ontario: a population-based study. Can J Psychiatry. 2017;62(10):716-725.
- Robbins, R . Will the coronavirus be a breakout moment for virtual mental health care? STAT. 2020 Apr 13. [accessed 2021 Sep 13]. https://www.statnews.com/2020/04/13/remote-mental-health-livongo-omada/.
- Uscher-Pines, L. et al. Use of tele-mental health in conjunction with in-person care: a qualitative exploration of implementation models. Psychiatr Serv. 2020;71(5):419-426.
Interested in learning more?
Interested in partnering with us or learning more about
what we can offer you? Please reach out here.
Get the latest resources and insights
-

eReferral and Aging Populations
Communication between providers and patients is crucial to providing effective patient-centered care. The aging population…
-

Patient experience with eReferral in Ontario Health West Region
Patients who receive appointment information and reminders through eReferrral, report an improved healthcare experience and…
-

A case study on the impact of the heart failure EMR tool in primary care
Heart failure is a chronic condition with a high risk of death. Once diagnosed with…
-

How AI scribes enable better interactions with patients during appointments
AI scribes are improving patient-clinician interactions by reducing administrative tasks, allowing clinicians to be more…